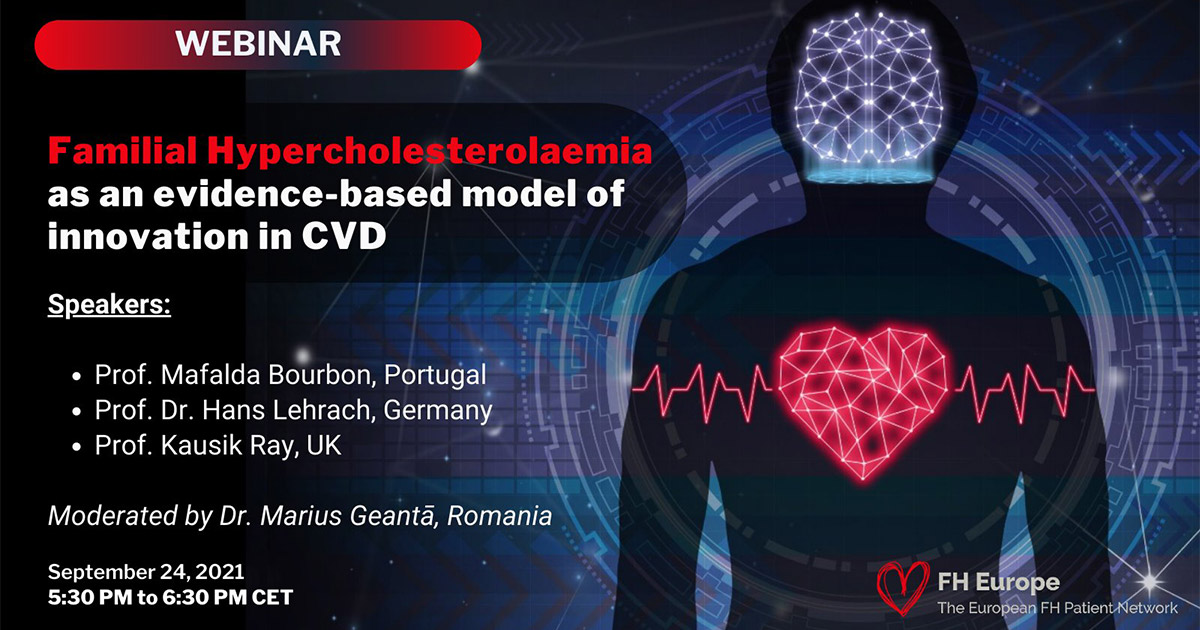
#FHAwarenessDay Webinar: familial hypercholesterolemia, a model for innovation in cardiovascular disease prevention
On September 24, The European FH Patient Network (FH Europe) organized a webinar in the context of the FH Awareness Day, “Familial Hypercholesterolemia: a model for innovation in CVD prevention”.
Familial hypercholesterolemia (FH) is e genetic disorder that causes premature cardiovascular disease and has been recognized as a public health priority. Worldwide, 90% of cases are undiagnosed. However, emerging technologies are changing life expectancy and quality of life for FH patients and their families. The discussion aimed to set the scene on how to imagine the future of FH and move towards truly personalized prevention in CVD.
The webinar gathered high-level international speakers, experts in cardiology, public health, and genomics:
- Mafalda Bourbon, Head of R&D Unit and Head of Cardiovascular Research Group, Department of Health Promotion, INSA
- Hans Lehrach, one of the pioneers of the Human Genome Project, former Director at the Max Planck Institute for Molecular Genetics
- Kausik Ray, EAS President and Director of the Imperial Centre for Cardiovascular Disease Prevention, Imperial College London
The discussion was moderated by Dr. Marius Geanta, Co-Chair of the Scientific and Public Health Advisory Group, FH Europe, and President of the Centre for Innovation in Medicine.
The value of innovation in changing paradigms in CVD
From a scientific perspective, we already have all the tools to aim for translating research into better outcomes for people, and avoid the consequences of “one-size fits all approaches”:
“We need to rethink medicine towards evaluating a single individual. Each of us is biologically different and that is why we must move towards personalized prevention. We need new models for prevention – in other areas we have made the transition to using computer models to simulate errors. We have virtual twins (Digital Twins) of airplanes, and we should also have this model in the medical field. Therapies that are not customized for the patient are associated with many adverse effects.” – Prof. Hans Lehrach
To ensure equitable access to such innovations, new models for public health are required:
“I see innovation as a facilitator for larger projects. We have the commonest genetic affection affecting mankind, with a prevalence of 1:311. Without innovation we cannot find these people and change their lives and prevent disastrous consequence.“ – Prof Kausik Ray, EAS President
“Each person is unique and should be treated accordingly. Current technologies and available data allow us to rethink medicine, including cardiovascular disease and cardiovascular prevention. (…) We are at the point where we need to work with FH and move towards pediatric screening. Current data indicate that diagnosis should be made 20-30 years earlier, from childhood. This aim to diagnose and detect early makes us move inevitably towards the era of genetics, genomes, humanities, innovation in public health.” – Dr. Marius Geantă

Diagnosing FH: 40 years of missed opportunities
A new study, published on September 9 in The Lancet, included findings from the European Atherosclerosis Society (EAS) Familial Hypercholesterolemia Studies Collaboration (FHSC) Global Registry of over 42,000 individuals from 56 countries. This type of data is crucial for driving changes in health policy across the globe for FH, a common genetic condition.
“Policymakers do not change if they do not see data. Individually, a country might say they don’t have data. When you put the global data together that data have power. We started the registry in 2015 with a simple vision: standardize how data is collected. There were countries with no data collection. The idea is in time each country will have enough expertise to be independent. We started collecting, and refining data. Now, this is a living, breathing organic data set that will grow and I want to thank all my colleagues around the world for contributing”
The results show that FH is underdiagnosed and undertreated:
- At the entry in the Registry, one in six people already had heart disease. FH was diagnosed with a delay of 4 decades, which means many missed opportunities;
- As many as 40% of patients do not receive treatment. There are also gender differences: women were less likely to receive lipid-lowering treatment.
- Less than 3 % of patients on treatment attained LDL-C levels recommended by the guidelines (<1.8 mmol/L);
“FH occurs in all regions of the world, irrespective of ethnicity, color, gender. We are diagnosing FH – a condition present from birth – in the mid-40s, women later than men. Less than 2% are diagnosed before the age of 20. If you start treatment early you can normalize the life course. We miss 45 years of cholesterol exposure. As the age of diagnosis increases, the prevalence of CVD also increases and the prevalence of risk factors.“ – Prof. Kausik Ray
Globally, when lipid-lowering therapies are used, 80% of patients receive monotherapy. Combined therapies are used in less than 20% of cases. FH patients need combination therapies and the number of innovative therapies increases every year.
“We can normalize LDL exposure but we need to gain those 30 – 40 years of treatment. We‘ve got the tools, we have to put systems in place, we need to implement it. We have the infrastructure to do genetic and genomic screening. We must address inequalities and we need policy makers to put money behind and screen.“
The real opportunity is to find children with subclinical disease before the consequences appear. According to Prof Ray, the key is starting early: “If you start early, you get a bigger return. This is critical for our politicians to understand.”
Towards zero CVD events in FH patients. The role of multi-omics
The diseases that cause the greatest global burden, such as CVD, are multifactorial. It is estimated that up to 75% of premature CVD is preventable. Traditional CVD management is largely aimed at changing lifestyle-related factors. However, advances in genomic medicine allow for a more comprehensive approach: accurate diagnosis, improvement in risk stratification, and targeted treatment. The value of precision medicine is defined by all the data that can be generated about an individual. Advances go beyond isolated clinical data, imaging or classical laboratory tests, toward the integration of more complex data sets (genomics, metabolomics, proteomics and so on), sometimes called “panomic profiling”. The applications of genomics and emerging sciences have the potential to revolutionize the prevention, diagnosis, and treatment of cardiovascular diseases, following the model that already revolutionized oncology.
“We have proposed a model for personalized medicine: from phenotype to genotype to treatment. We can identify several distinct diseases under the phenotype of familial hypercholesterolemia if we use genomics but also metabolomics, transcriptomics. The idea is to use the omic sciences to understand familial hypercholesterolemia. We’re at an important stage of technology, with each day we are more precise and that’s extraordinary. Patients can be identified earlier and treated correctly. I think the goal is to get to zero cardiovascular events in people with FH” – Prof. Mafalda Bourbon
The development of genomics allowed informed decisions around treatment options for FH. There are 3 main genes involved in FH (LDLR, PCSK9 and APOB), the most common mutations are found in the gene coding for the LDL receptor, the most important protein to clear LDL from the circulation. Prof. Bourbon explained that it is possible to precisely determine the activity of this receptor, which is valuable information that can guide treatment:
“There are mutations that slightly affect the LDL-R activity. For those, an optimal strategy is using statin and ezetimibe to reduce the high risk of the patients. In other patients, there is no LDLR activity, and a more aggressive strategy is needed, with 3 or 4 different drugs. We have those in the market already. FH has this wonderful scenario: you identify the patient by genetics and genomics approaches, and then which is the best treatment.”
However, in 50% of patients with a clinical diagnosis of FH, a causative mutation is not found in one of those 3 genes. In such cases, it is essential to perform further analyses to understand the metabolic pathways (metabolomics), the protein function (proteomics) or even identify different, new genes. In some cases, there is a polygenic component involved.
“They don’t have to have FH, they have a dyslipidemia. Using this kind of integrated analyses, we find new disorders of lipid metabolism. The FH phenotype can hide other phenotypes.“ – Prof. Bourbon
Beyond the deep understanding of disease biology, nowadays, true personalization also means a better evaluation of the person behind the diseases: “We are different not just because the genomes are different, but because we behave differently. This is why is important to integrate essential data about a person. (…) Personalized medicine is the only way to achieve effective healthcare” – Prof. Hans Lehrach
The debate around new models for prevention will continue in the following months, with CVD gaining a spotlight in the health policy agenda of Europe.
Upcoming events:
- September, 27
Join the Launch of the European Alliance for Cardiovascular Health, an initiative aiming for a common EU policy approach to cardiovascular diseases for the benefit of the citizens. The event will gather the founding organizations of the European Alliance for Cardiovascular Health (including FH Europe, ESC, Global Heart Hub, EFPIA, MedTech Europe), representatives of the European Commission, Member States and European Parliament.
- October, 11
In the context of the Slovenian Presidency of the Council of the European Union 2021, a technical meeting on Achieving Equity and Innovation in Newborn Screening and in Familial Hypercholesterolemia Paediatric Screening across Europe will be organized in a virtual format. The meeting aims to address the fundamental challenges and opportunities to achieve equity of access to FH screening across Europe, to identify best practices in the field of FH pediatric screening and how they could be replicated and taken to scale, and also to agree on the next steps to ensure a systematic and comprehensive approach to screening in Europe that leaves no-one behind. The event is endorsed by many international societies including FH Europe and the Centre for Innovation in Medicine.

